
Migraine, a Dance of Harmony and Havoc
Zsofia Hesketh is an interdisciplinary scholar and public health professional with a background in philosophy, medical research, and clinical medicine. She is completing her MSc Translational Medicine as a visiting student at Sorbonne Médecine, Paris, where she is focusing on gynaecology and neglected aspects of women’s health.
This article is part of the intersections theme.
edited by Kenia & heini, reviewed by tiina paakkunainen, illustrated by vasiliki gniki.
Once upon a time, in the intricate network of the human nervous system, there existed a cranial nerve known as the trigeminal nerve. One of the largest nerves in the head, it possessed the power to carry sensory information from the face and neck to the brain, including touch, pain, and temperature sensations. Literally meaning ‘thrice-twinned’, its name was chosen in reference to its three pairs of branches leading to the ophthalmic, maxillary, and mandibular areas – that is, the forehead and eye zone, the upper jaw and cheek zone, and the lower jaw and chin zone of the face. A multitalented fellow, the trigeminal nerve also revealed its role in facilitating local motor functions, such as biting and chewing. A marvelous system indeed, but one which would soon go into disarray during migraines, as its once harmonious functioning took an unexpected twist. To understand this better, we’ll need the assistance of modern medical science…
…right, back to the twenty-first century. In the world of migraine, there exists a delicate balance between excitement and inhibition. For this third article of the mini-series on sex-sensitive medicine, I invite you to unravel with me the enigmatic and hormone-influenced story of migraine, a type of one-sided headache which, for reasons not yet clear, occurs 2-3 times more frequently in women than men.
How Migraines Begin…
Every story needs a trigger, and in the case of a migraine, it can start with several internal or external factors. These factors include stress, hormonal changes, certain foods, or environmental stimuli like sunlight and air quality. The specific trigger or combination of triggers differs from person to person and even from occasion to occasion. What is true across the board, however, is that triggers set the stage for a cascade of events within the brain. The result, you ask? A large serving of debilitating pain and a variety of sensory or motor symptoms as sides.
The first dominos to fall are the blood vessels, whose dilation is fueled by the release of powerful substances with “easy-to-retain” names like “calcitonin gene-related peptide” (CGRP) and “substance P”. To understand this better, imagine that your brain is a balloon, and the blood vessels in your brain are the balloon’s walls. At resting state, the balloon is limp, essentially collapsed. However, this changes when the ‘trigger’, in this case, a sudden gust of air being blown into the balloon, causes the walls to expand and stretch, widening their diameter. This is akin to the change in the state and shape of the blood vessels in the brain provoked by one of the headache triggers mentioned above. As vessel walls stretch, they become thinner, more sensitive, and inflamed, much like how a balloon’s walls become translucent, thin, and prone to bursting when overfilled with air. When the blood vessels’ walls expand, they become more permeable, allowing inflammation-causing molecules called ‘cytokines’ to enter and exit more freely. Cytokines, taking advantage of the porousness of vessel walls, travel through the blood to the brain’s membranes (‘meninges’), causing painful irritation both in these membranes and in the trigeminal fibres connected to them. It is during this phase that our hero of the story, the trigeminal nerve, is disturbed from its normal functions. Think of it as a kid (a cytokine) starting to poke you (the nerve) with their finger, multiplying into a hundred kids, all poking you at the same time. This is bound to go from frustrating but painless to complete sensory overload. At this point, pain perception is heightened in surrounding trigeminal nerve fibres, which transmit these electrical signals to the brain to invoke the throbbing, pounding, or stabbing sensations that migraine sufferers know all too well. However, before culminating in pain, these frenzied waves of electrical signals may first engender ‘aura’.
Aura, a Kaleidoscope in the Brain
Aura is an umbrella term for migraine-associated neurological disturbances like visual spots, tingling sensations, and even a temporary loss of speech (American Headache Society). In the figure below (Fig.1), you can see some examples of how visual aura may manifest in the eyes of the sufferer. Quite a range, right?
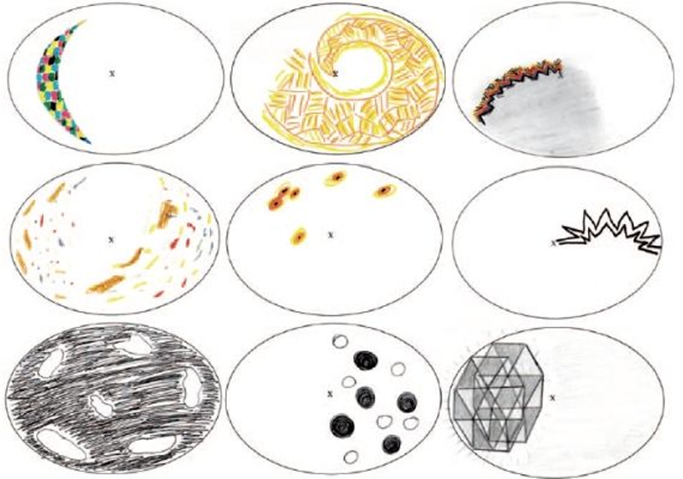
The exact way that nervous signalling leads to aura is not fully understood, but it has been found to be associated with an increased risk of stroke, especially in female sufferers. Typically, an aura lasts for 10 minutes to half an hour and then fades away as the migraine pain begins. Meanwhile, light and sound sensitivity symptoms can accompany and persist for much of the duration of the headache phase, requiring patients to lie in dark, quiet rooms. If you wish to put yourself in a migraine sufferer’s shoes, these testimonials vividly illustrate the disorientation and incapacitation caused by the condition, including the following experience:
“It felt like my skull couldn’t accommodate the balloon that someone was blowing up inside of my head.”
“Pain and pressure that radiates down to my eye… I felt like I couldn’t keep track of the road, like it was moving away from me.”
“That one time I had a migraine so severe they did not know whether it was a migraine or a stroke”.
Theories and Discoveries Around Migraine Risk in Women
As for why migraine is more common in women, especially women of childbearing age, the full explanation remains to be uncovered. Approximately 50% of female migraine patients have attacks during specific times of their menstrual cycle with up to 20% experiencing so-called “pure menstrual” migraines, migraines that occur between days -2 and +3 from the onset of menstruation. From these patterns, it is inferred that fluctuations in the female sex hormone oestrogen, which is secreted by the body at various levels throughout the menstrual cycle, play a role (for more information, see my previous article on female reproductive hormones). This is because oestrogen is thought to alter the balance of chemicals involved in regulating blood vessel width and pain perception. For example, there is tentative evidence that oestrogen levels are negatively correlated with levels of CGRP mentioned above.
A recent review from Charité University Hospital, Berlin, found that female migraine patients have significantly higher concentrations of CGRP (which, remember, is a molecule involved in blood vessel dilation) during menstruation than healthy women. It is hypothesised that this is related to the drop in oestrogen levels directly preceding and during the first few days of menstruation, which begs the (still unanswered) question of whether the migraine-suffering women had a more dramatic decrease in the hormone than their counterparts. In other words, the sudden decrease in oestrogen seems, whether directly or indirectly, to inversely increase the production of CGRP, engendering a withdrawal syndrome of sorts.
This could also explain why women appear to experience more migraines and headaches in other low oestrogen states. This includes the post-partum period, when a significant decrease in oestrogen occurs once the placenta is delivered; the transition to menopause; and the period following a hysterectomy, an operation to remove the uterus (and sometimes the oestrogen-producing ovaries) for cancer treatment, sterilisation or other purposes. To summarise, migraine may become more likely in various states of ‘oestrogen withdrawal’ as a result of an associated increase in CGRP levels. Whether this can only occur in combination with a triggering stimulus or whether this mechanism comes first and sensitises patients to potential triggers is currently unknown. To complicate things further, other substances also seem to mess with blood vessel dilation and pain perception, like the neurotransmitter serotonin, which adds an extra layer of mystique to the mechanism behind this debilitating condition.
More detailed investigations into how migraine risk changes throughout the menstrual cycle are needed to shed light on this hormone’s influence. Especially, closer comparisons between healthy and migraine-suffering women are warranted to determine any differences in their hormonal or lifestyle profiles. The picture is further complicated by the fact that the most common form of contraception, the combined oestrogen-progesterone pill, is a severe risk factor for stroke in women with aura migraines. On the other hand, it also stabilises hormone levels throughout the cycle, thus seeming to reduce migraine occurrence in those with ‘regular’, non-aura attacks. This delicate interaction, while widely known by health professionals, is still sometimes overlooked by less perceptive or attentive clinicians when prescribing the pill.
Towards a Sex-Informed Research Model
In truth, as you can see, a migraine is much more than just a headache. It is a complex and sometimes debilitating condition of which headache is but one of many dimensions. Other common symptoms include sensitivity to light and sound, nausea, and trouble focusing or concentrating. Just as it is symptomatically complex, migraine can strike in unpredictable patterns, varying from once every few years in one person to several times a week in another.
Much remains to be learned, including a differentiated approach to researching female-specific migraine causes, pathways, and treatment strategies. A more immediate target is for physicians to take their patients’ pain more seriously and to pay close attention to dangerous interactions when discussing contraceptive options. Turning to the research community, we will only stand a chance at uncovering sex-specific pathways in migraine if female animal models are included in future studies. This gap in scientific methodology was highlighted in the introductory article for this series and will be emphasised further in our next article, an interview with Dr. Maddalena Ardissino on the knowns and unknowns of women’s cardiovascular health.
references
Aggarwal, M., et al. “Serotonin and CGRP in Migraine.” Annals of Neurosciences, vol. 19, no. 2, 1 Apr. 2012, www.ncbi.nlm.nih.gov/pmc/articles/PMC4117050/, https://doi.org/10.5214/ans.0972.7531.12190210.
American Headache Society. “Aura with Headache”.URL: https://americanheadachesociety.org/wp-content/uploads/2018/05/Aura-With-Headache-June-2014.pdf
Brandes J. “The influence of estrogen on migraine: a systematic review.” JAMA. 2006. Vol. 295 1824–1830. DOI: 10.1001/jama.295.15.1824
Huff, T. et al., “Neuroanatomy, Cranial Nerve 5 (Trigeminal).” PubMed, StatPearls Publishing, 2022, www.ncbi.nlm.nih.gov/books/NBK482283/#:~:text=The%20trigeminal%20nerve%20is%20the.
Jacobs, B., and Dussor, G. “Neurovascular Contributions to Migraine: Moving beyond Vasodilation.” Neuroscience, vol. 338, Dec. 2016, pp. 130–144, https://doi.org/10.1016/j.neuroscience.2016.06.012.
Kesserwani H. “Migraine Triggers: An Overview of the Pharmacology, Biochemistry, Atmospherics, and Their Effects on Neural Networks”. Cureus. 2021 Apr 1;13(4):e14243. doi: 10.7759/cureus.14243
Mancall, E. et al., “Gray’s Clinical Neuroanatomy: The Anatomic Basis for Clinical Neuroscience” 1st Edition. 2011.
Martin, V. and Behbehani, M. “Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis–part 2”. Headache. 2006;46:365–386. DOI: 10.1111/j.1526-4610.2006.00370.x
Mason, B. and Russo, A. “Vascular Contributions to Migraine: Time to Revisit?” Frontiers in Cellular Neuroscience, vol. 12, 3 Aug. 2018, https://doi.org/10.3389/fncel.2018.00233.
Migraine Canada. “Migraine with aura: an overview” URL: https://migrainecanada.org/posts/the-migraine-tree/roots/migraine-categories/migraine-with-aura-an-overview/
Moy, G. and Gupta, V. “Menstrual Related Headache.” PubMed, StatPearls Publishing, 2021, www.ncbi.nlm.nih.gov/books/NBK557451/.
Raffaelli B et al. Sex hormones and Calcitonin Gene-Related Peptide (CGRP) in women with migraine: a cross-sectional, matched cohort study. Neurology 2023 Feb 22. doi: 10.1212/WNL.0000000000207114
Sacco, Simona, et al. “Migraine in Women: The Role of Hormones and Their Impact on Vascular Diseases.” The Journal of Headache and Pain, vol. 13, no. 3, 26 Feb. 2012, pp. 177–189, https://doi.org/10.1007/s10194-012-0424-y” https://doi.org/10.1007/s10194-012-0424-y.